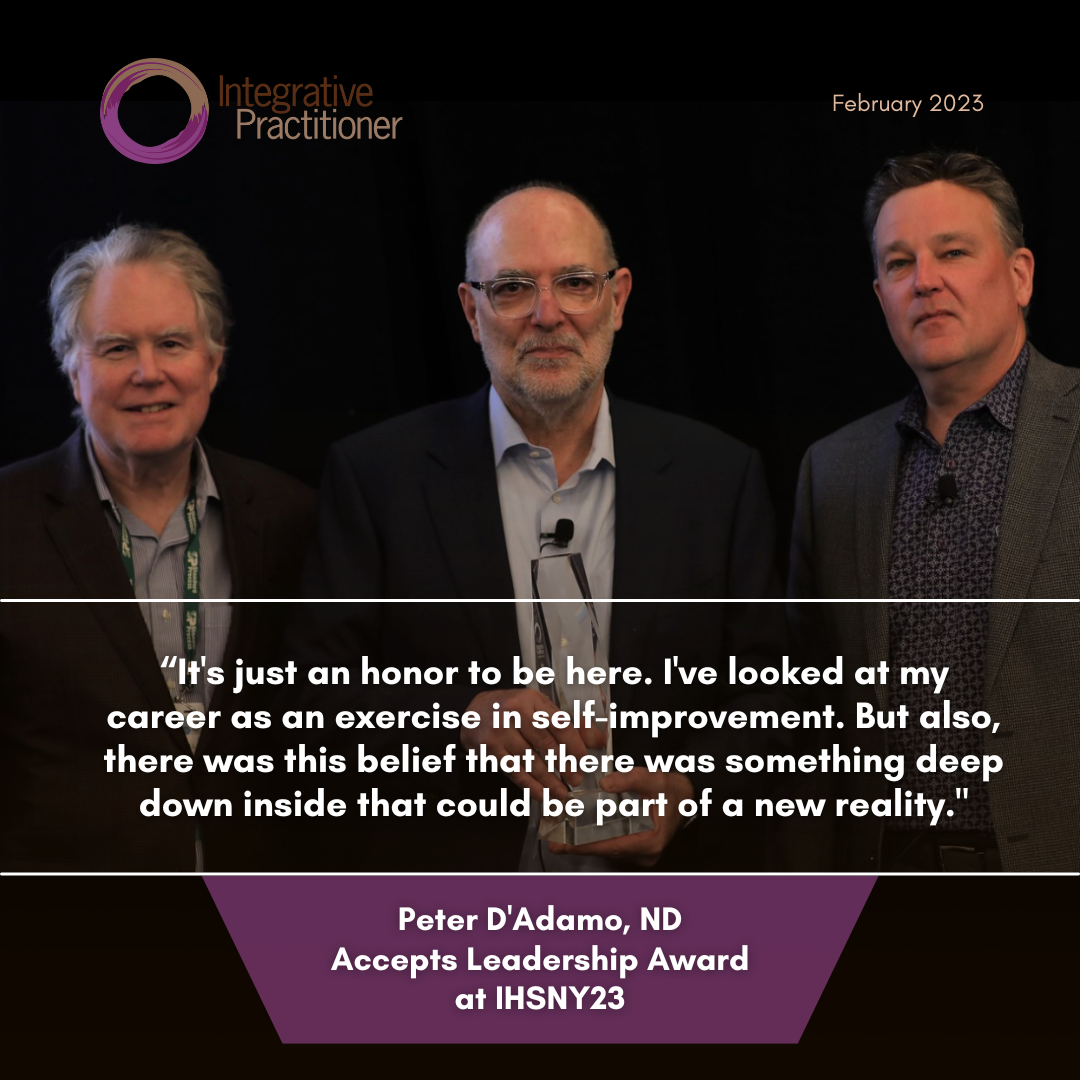
The Integrative Healthcare Symposium awarded Peter D’Adamo, ND, as the recipient of its 2023 Leadership Award, which was presented to him today during the Integrative Healthcare Symposium in New York City.
The Leadership Award recognizes a pioneer whose contributions have shaped integrative healthcare and paved the way for other practitioners and professionals. This year, David Brady, ND, DC, CCN, DACDN, IFMCP, FACN, chief medical officer for Diagnostic Solutions Labs, presented the honor.
Notable past recipients include Andrew Weil, MD, David Perlmutter MD, FACN, ABIHM, Joe Pizzorno, ND, Mark Hyman, MD, and Tieraona Low Dog, MD.
LEARN MORE